Cardiography
Learning Objective
- Basic Function of the Heart
- Physiological Measurements
- Heart Electrical Stimulators
- Basic Electrical Safety
Heart
Basic Function
The heart is the pump station of the body and is responsible for circulating blood throughout the body. It is about the size of a clenched fist and sits in the chest cavity between the two lungs. Its walls are made up of muscle that can squeeze or pump blood out every time that organ “beats” or contracts.
Fresh, oxygen-rich air is brought to the lungs through the trachea or every time that you take a breath. The lungs are responsible for delivering oxygen to the blood, and the heart circulates the blood to the lungs and different parts of the body.
The heart beats’ about 100,000 times in one day and about 35 million times in a year. During an average lifetime, the human heart will beat more than 2.5 billion times. The body has about 5-6 litres of blood around it three times every minute. In one day, the blood travels a total of 19,000km. The heart pumps about 1 million barrels of blood during an average lifetime - thats enough to fill more than three super tankers!
Functional Anatomy of the Heart
The human heart consists of four “chambers” - two atrial and two ventricular cavities which are separated by muscle walls and valves. The main function of the heart is to be a pump but actually it acts as a double pump - right and left. The right pump sends blood into lungs for oxygenation. The left pump supplies the whole body with oxygenated blood (it is more powerful). Together with muscle cells, the heart wall contains specialised cells which form a network allowing an electrical impulse to spread through the heart.
Blood Circulation through the Heart
- Blood returns in the heart from system circulation to the right atrium (through the vena cava)
- From the right atrium it travels to the right ventricle (through the tricuspid valve)
- From the right ventricle it is ejected to the lungs (through the pulmonary artery)
- From the lungs the oxygenated blood returns to the atrium (through the pulmonary vein)
- From the left atrium it goes to the left ventricle (through the mitral valve)
- From the left ventricle the oxygenated blood is ejected to the system circulation (through the aorta)
Excitatory and Conductive System of the Heart
The heart is composed of three major types of cardiac muscle: atrial muscle, ventricular muscle and specialised excitatory and conductive fibres. The atrial and ventricular muscles are very similar to skeletal muscle by its structure but the duration of contraction is much longer.
The heart structure includes a specific system for generating rhythmical impulses to cause rhythmical contraction of the heart muscle. The conductive system delivers these impulse rapidly throughout the heart muscle.
Heart Excitation and Contraction
- The sinoatrial (SA) node includes self-excitatory pacemaker cells. They generate pulses at a rate of ~70/min.
- These pulses propagate through the atria, but can not go to the ventricles.
- The atrioventricular (AV) node is between the atria and ventricles and has an intrinsic frequency of 50 pulse per min.
- However AV node can be triggered at a higher frequency - i.e. normally it follows the pace of the SA node
- Pulse propagation from the AV node to the ventricles is made through specialised conduction system
- This system provides the pulse at relatively high speed to the ventricles (through the Purkinje fibres)
- From the inner wall of the ventricles the many activated fibres create a wave front which propagates through the ventricular mass toward the outer wall of the muscle and causes contraction (pumping).
- After each activation, de-activation occurs and the muscles are ready for a new activation pulse.
Formation of an action potential
- Neurons communicate through nerve action potentials (impulses) based on electric current of ions
- Generation of action potential depends on: ion channels in cell membrane & resting membrane potential
- In the rest the cell is polarised - its membrane has internal negative potential (~approx. -70 mV) in respect to the extracellular space (inside there are mainly PO43- ions, and outside mainly Na+ ions; K+ ions flow-in-out)
- An external stimulus can open some ion channels in cell membrane (N.B. Na channels open first) allowing Na+ ions to enter the cell thus making it positive (up to +30 mV) - action potential (Depolarisation)
- Some time after opening of Na channels, the K channels open (increased membrane permeability for K), and K+ ions flow out, restoring the initial negative polarisation inside the cell (Repolarisation)
- The impulse from one cell stimulates the channels in the adjacent cell, this way propagating the stimulus.
- The size of the impulse is independent of the strength of the stimulus. After the repolarisation the cell has a refractory period, during which it restores its ionic balance and cannot be stimulated again.
An action potential (AP) is a rapid change in the membrane potential during which the potential rapidly depolarises and repolarises. The potential reverses and the membrane becomes positive inside. AP provides long-distance transmission of information through the nervous system. Half or more of all smooth muscle contraction is initiated not by actions potentials nut by stimulatory factors acting directly on the smooth muscle contractile machinery. The two types of non-nervous and non-action potential stimulating factors most often are:
- Local tissue factors: lack of oxygen in the local tissue and an excess of carbon dioxide causes smooth muscle contraction
- Various hormones: most of the circulating hormones in the body affect smooth muscle contraction (these include serotonin, histamine, epinephrine, oxytocin).
There are two major differences between the membrane properties of the cardiac and skeletal muscle:
- The action potential of skeletal muscle is caused by sudden opening of large numbers of “fast sodium channels”. In cardiac muscle, the action potential is caused by the opening of two types of channels: “fast sodium channels”, which are the same as in skeletal muscle, and “slow calcium-sodium channels”, which are much slower.
- Immediately after the onset of the action potential the permeability of the cardiac muscle membrane for potassium decreases about five times. This process does not occur in skeletal muscle. The decreased potassium permeability greatly decreases the outflow of potassium ions during the action potential plateau and thereby prevents early recovery.
The duration of the plateau ensures cardiac contraction which lasts 20 to 50 times longer than in skeletal muscle. The refractory period of atrial muscle is much shorter than for the ventricles (about 0.15 second) and the relative refractory period is another 0.03 second. Therefore, the rhythmic rate of contraction of the atria can be much faster than that of the ventricles.
The surface of cardiac muscle is oppositely polarised compared with inside cells
Physiological Measurements
After imaging, physiological measurements are among the most important diagnostic methodologies used in health care.
Electrocardiogram ECG
The body fluids are good conductors, fluctuations in potential that represent the algebraic sum of the action potentials of myocardial fibres can be recorded from the surface of the body. The rocked of these potential fluctuations during the cardiac cycle is called ECG.
The phase of ECG formation, based on the changes of the summary potential (vector) of the cardiac surface. The bulk electrical activity of the heart produces a reasonable sized signal on the body surface, which can be measured by connecting electrodes to the skin. The recorded waveform and amplitude (1 mV) depends greatly on the position of the electrodes.
The P wave is caused by the atrial depolarisation prior to contraction.
The QRS complex (~ 1mV amplitude) is caused by currents generated when the ventricles depolarise prior to contraction. Therefore, both P wave and the components of the QRS complex are depolarisation waves.
The T wave is caused by currents generated as the ventricles recover from the state of depolarisation.
Registration of the ECG
The yellow electrodes are attached to the left arm and the red electrodes to the right arm, green to the left leg and black to the right leg (ground electrode).
Horizontal and vertical calibration is made using a grid printed or display. The horizontal lines are the voltage, 10 small divisions upward or downward represent 1 mV. The vertical calibration lines represent the time, with each 2.5 cm representing a second. The standard speed is 25 mm/s.
ECG abnormalities
There are many different heart abnormalities that can be picked up with an ECG:
- Arrhythmia is the change of the normal sinus rhythm due to defects in conduction of the cardiac impulse.
- Heart block is when the conduction system between the atria and ventricles fails.
- Bradycardia is the slowing of the heart rate
- Tachycardia is an elevated heart rate
Other ECG leads
The electrical activity of heart forms isopotential lines over the body surface, which assume various positions of ECG leads (with different signal waveforms).
Blood Pressure
As blood is pumped out of the left ventricle into the arteries the pressure in the aorta rises, the higher level being the systolic pressure. At the end of the left ventricular contraction, blood flows away from the heart so the aortic pressure falls. When the aortic valve closes, a notch appears on the pressure waveform. The lowest pressure is just before the next heartbeat, and is the diastolic pressure. The rate at which pressure falls depends on the systemic vascular resistance (SVR).
MAP - Mean Arterial Pressure, CO - Cardiac Output, SVR - Systemic Vascular Resistance, CVP - Central Venous Pressure
Mean Arterial Pressure (MAP) is the average pressure in a cardiac cycle. It is not the value halfway between systolic and diastolic pressures because the diastole lasts longer than systole (470 vs 330 ms).
Blood Pressure Measurement
In 1904 Korotkoff described the sounds that blood made as it moved intermittently through an artery when measuring blood pressure. The artery distal to the cuff is listened to using a stethoscope (auscultation method).
- The first sound appear (is hear in the stethoscope) when the cutoff pressure falls below the peaks of blood pressure and blood can flow intermittently in the artery (systemic pressure)
- As the cuff pressure drops below the diastolic pressure, blood flows continuously, the artery walls no longer close and the sounds of intermittent blood flow (heard in the stethoscope) disappear
Auscultatory Method
Measuring the ABP (arterial blood pressure) using the auscultatory enables the doctor to find a few different variables:
Systolic Pressure (SP) is the maximum pressure reached during peak ventricular ejection. Normal values at rest - between 100 and 140 mm Hg.
Diastolic Pressure (DP) is the minimum pressure reached during ventricular relaxation. Normal values at rest - between 60 and 90 mm Hg.
Pulse Pressure (PP) is the difference between the systolic and diastolic pressure. PP = SP - DP
Heart Electrical Stimulators
Programmable Pacemaker
Cardiac Pacemaker is an electric stimulator that produces periodic small electrical pulses to the heart (as from the AV and/or SA nodes). The stimulus aims to generate heart contraction (atrial and/or ventricular)
Approximately 500,000 new pacemakers are implemented each year and other 100,000 are replaced
There are two main types of pacemakers:
1. Competitive
This is a fixed rate (asynchronous) pacemaker.
2. Non-competitive
This is split into another two types, depending on the location. There are ventricular pacemakers that are either R-wave inhibited (demand) or R-wave triggered. And there are Atrial pacemakers that are usually P-wave triggered.
How a Pacemaker works
A Pacemaker has to work in synchrony with the heart natural pace, or to fully replace it. If it works in synchrony it has to detect the main heart rhythm (R wave) and, if R wave is there to inhibit the internal timer, but if it is different from the expected one, to generate a stimulus pulse (Feedback 1). The amplitude and duration of the stimulus electrical pulse can change to deliver the needed effect.
The pulse parameters depend on the the battery of the pacemaker. Feedback 2 constantly monitors the battery output and modifies the pulse parameters to deliver the needed effect. The pacemaker has to be protected from external strong electrical fields/pulses (e.g. Defibrillator). A number of leads (electrodes) deliver the pulse to the heart (same leads measure the heart activity).

Electrodes (either unipolar of bipolar) deliver a 1 millisecond pulse with 10 mA amplitude to the heart. The lead must survive constant flexing (30 - 40 million cycles per year) in warm, corrosive saline medium, therefore it is made out of platinum with 10% iridium alloy.
External pacemakers are for temporary arrhythmias and internal pacemakers are implanted for more permanent conditions.
The electrodes have a tissue resistance of ~500 Ω. Therefore using the P = I2R equation:
1 sec x 50mW will give average consumption of 50 μW per second (at 60 bpm). 10 mA flows for 1 msec - what gives an average of 10 μA per second.
The battery capacity (mAh) has to supply these 10 μAs for a number of years. Useful battery capacity divided to pulse charge 10 μAs will give the useful period of function (usually more ~ 10 years). This period depends on the type of use and the type of battery (i.e. lithium iodine cell).
Defibrillator
A defibrillator is an electrical device that produces a strong electrical pulse to heart aiming at re-establishing a more normal cardiac rhythm.
Atrial Fibrillation is where the ventricles still function but with an irregular rhythm.
Ventricular Fibrillation is very dangerous as the pumping function of ventricles stops.
Defibrillators deliver large electric shocks to the heart aiming to restore a normal sinus rhythm: total stop of the heart which inhibits fibrillation in hope that the heart will re-start in an orderly rhythm. The position of the electrodes is crucial for this to work.
The resistance of the skin/electrodes is ~50 Ω and the current through the chest is ~ 50 A. Pulse duration is ~ 4 msec.
Block Diagram of a Defibrillator

Inside the fibrillator is a capacitor which discharges itself over the heart.
There are three main types of defibrillators:
- Direct (during surgery) - max output ~ 50 J
- Cardioversion (synchronised clock across the chest for atrial fibrillation) ~20-200 J
- Emergency (ventricular fibrillation) - first pulse of ~200 J followed by higher E.
Implanted defibrillators (max 30 J) has a battery that is sufficient for ~ 100 shocks.
Basic Electrical Safety
A macro shock is where a high current passes through the body with a small component passing through the heart. A micro shock is a low value current passing directly through the heart.
Physiological effects of electricity
Tissue heating > x.10 kHz
This results at all frequencies if the power density is high enough.
Neuromuscular stimulation from x Hz to x kHz
Alternating current stimulates muscles directly. Ventricular fibrillation threshold is high for short impulses (e.g. 2 A for 200 msec) but fails dramatically for pulse durations approaching 1/3 of the cardiac cycle). Stimulation can occur through the skin:
- 1 mA: threshold of sensation
- ~ 6 mA: Let-go current is the maximal current at which the subject can withdraw voluntarily (before muscle paralysis)
- 18 - 22 mA: respiratory arrest
- 75 - 400 mA: ventricular fibrillation
- 1 - 6 A: sustained myocardial contraction
- Greater than 10 A: burns
Direct heart stimulation - ventricular fibrillation threshold is very low (~60 μA at 50 Hz)
Electrolysis very low freq
This takes places at electrode-tissue interfaces (even at d.c.). If a current of 0.1 mA d.c. passes through an electrode to jelly to skin for ~x minutes it can causes an ulcer.
Leakage Current
In hospital electrical devices a ground wire takes leakage current proportionally to the difference of resistance ground/heart (in the case 10,000 times more μA). However if the ground wire is broken all 100 μA leakage current will go through the heart and a micro-shock occurs at 60 μA (50 Hz).
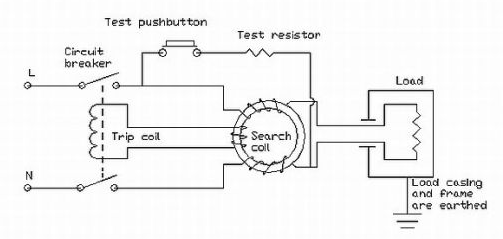
Earth Leakage Circuit Breaker ELCB
It monitors the balance of incoming and outgoing current flows (from Live and Neutral) and interrupts the circuits if an imbalance is detected.
Written by Tobias Whetton