Laser Optical Radiation
Learning Objectives
- The physics and different modes of operation of lasers
- Laser classification
- Quantifying laser hazards
- Protective eyewear
- Laser interactions
Introduction
We are interested in the following portion of the electromagnetic spectrum, regarding lasers:
| UV | Ultraviolet | 200 - 400 nm |
| VIS | Visible | 400 - 700 nm |
| NIR | Near Infrared | 700 - 1400 nm |
| MIR | Middle Infrared | 1400 - 3000 nm |
| FIR | Far Infrared | 3000 nm - 1mm |
Lasers created from an artificial optical coherent radiation source were first invented in 1960 by Maiman. LASER is an acronym for:
- Light
- Amplification by
- Stimulated
- Emission of
- Radiation
The basic components of a laser are:
- Laser medium: this determines the wavelength of the laser emitted and can be solid, liquid or gas
- Energy source: this gives energy to the laser medium which in turn emits light photons.
- Optical feedback: allows the light photons to interact (possibly many times) with the laser medium
Basic Laser Physics
Atoms in the losing material exist initially in the ground state with energy A.
Stimulated Absorption
An energy source source provides energy to the lazing material and *raises atoms from the ground state (A) to an excited state (A)** by a process called stimulated absorption. The energy required is A* - A, and the value of this depends entirely on the lasing material and determines the wavelength of the laser.
Population Inversion
The majority of the atoms in the lasing material are in the excited state.
Spontaneous Emission
Atoms spontaneously decay back to the ground state, emitting photons with random phase & direction.
Stimulated Emission
The “trigger photon” from spontaneous emission (with energy A* - A) encounters excited atoms from the lasing material. The excited atom is forced to emit a photon with identical direction & phase (i.e. wavelength) than the “trigger photon” leading to amplification.
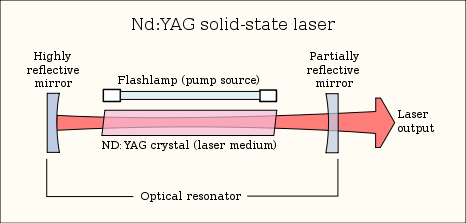
Laser Design
A lasing material is encased between two mirrors inside a laser cavity. An energy source excites the lasing material that emits photons. A back mirror is fully reflective & a front mirror is partially transmitting to allow photons to exit the laser cavity. The laser beam can only emerge when the shutter is opened (i.e. foot/hand switch activated). Beam delivery device directs the beam to its final destination. A cooling system is also required to maintain output level.
Beam Delivery System
The laser energy is transferred to the treatment site in one of two ways:
1. Articulated Arm
This hollow articulated arm has mirrors (highly polished stainless steel) at elbows. The beam alignment is crucial.
2. Optical Fibres
This uses reflections to trap the light inside (total internal reflection). Light rays can travel along glass or plastic fibres. The laser will lose it’s coherence (this has no significance for treatment purposes).
Laser Light Properties
Lasers have many different useful properties:
- Monochromatic (i.e. one frequency): all the light is emitted in a very narrow band of wavelengths.
- Coherent: all the light waves emitted from the laser are in the same phase (same wavelength and same frequency)
- Directional: laser light emitted is highly directional as it tends to diverge slowly.
- Intense: laser beams tend to have a high intensity, with some lasers up to x100 brighter than the sun.
Modes of operation
When treating a patient then the method of laser light delivery is very important:
- Continuous: Laser light is continuously pumped and continuously emits light.
- Pulsed: Laser is operated in short pulses which may be predefined or operator dependent. Typical pulse duration is 0.25 s to 10 μs.
- Q-Switched: Laser medium is pumped but the “trigger photons” that cause stimulated emission are prevented from entering the laser medium. Continued pumping leads to population inversion and gain saturation. At gain saturation, the “trigger photons” are allowed to enter the lasing medium resulting in emission of a giant pulse. Typical pulse duration is 5 - 40 ns.
Measuring Laser Output
Laser outputs tend to take into account the area of the beam as this is key to the effect the beam has on the surface. There are two main types of lasers, continuous and pulsed:
Continuous wave laser
For a continuous wave laser, power ($ \frac{energy}{time} $) is the most useful measurement, and its units are Watts (W). Irradiance takes into account the area of this power and it is measured in W/cm2
Pulsed laser
For a pulsed laser, energy is the most useful measurement, and its units are Joules (J). Radiant exposure (dose) takes into account the area of this energy and is measured in J/cm2.
Radiant Exposure (J/cm2) = Irradiance (W/cm2) x time
Interactions
Some of the properties become important when treating a patient.
Transmission
If no chromophore (an atom or group whose presence is responsible for the colour of a compounds) all photons will pass through the tissue without any effect. There will be total transmission. Selection of proper chromophore in or near the target is the first important step.
Reflection
This occurs at all interfaces of media, such as air, water, skin surface. Skin reflects 4% to 7% of visible light. To reduce reflection have firm contact with skin, light guide, US jelly, holding hand-piece perpendicular to the skin surface.
Scattering
This occurs predominantly from inhomogeneities in structures whose size is similar to the wavelength or slightly larger i.e. collagen fibres. It is the inverse function of wavelength. A shorter wavelength equates to greater scattering. The greater the scattering, the less depth of penetration and more possibility of absorption.
Other
Other factors also have a bearing on the depth of penetration. In tissues, more scattering occurs when a small spot size is used. With a large spot size, photons hit each other and are recollected and redirected downward increasing the depth of penetration.
Classification
A laser manufacturer is responsible for assigning all laser products to one of seven general hazard classes defined in BS EN 60825-1:2007:
| Class | Laser Type | Potential eye/skin hazard |
|---|---|---|
| 1 | Laser completely enclosed or Very low power level | Safe under all conditions in normal use |
| 1M | Low power level & large collimated beam diameter | Safe except when magnifying lenses are used |
| 2 | Low power level (<1 mW), Visible wavelengths only | Safe under accidental exposure (Blink reflex of 0.25s) |
| 2M | Low power level & large collimated beam diameter, Visible wavelength only | Safe under accidental exposure (Blink reflex of 0.25s) except when magnifying lenses are used |
| 3R | Low power level (<5 mW) | Accidental exposure not hazardous but eye injury possible for intentional exposure |
| 3B | Medium power (<500 mW) | Direct beam dangerous to eye, Diffuse/scattered light safe |
| 4 | High power (>500 mW) | Direct and diffuse/scattered light dangerous to eye & skin, Fire hazard |
Access to areas in which Class 3B or Class 4 lasers are used must be marked with warning signs.
Accesible Emission Limit
This determines the classification of a laser or laser product. It depends on how much access an individual has under normal operating conditions, for example:
- Open beam laser - full access - maximum hazard
- CD player - no access
- Laser printer - no access
Quantifying Laser Hazards
Maximum Permissible Exposure MPE
Maximum exposure level to laser radiation that (in normal circumstances) should not injure the eye or skin. Data and equations are given in BS EN 60825-1:2007
It is at a different value for the skin and the eyes. MPE can be stated in two ways discussed earlier:
- Watts per metre squared (W/m2) is termed ‘Irradiance’
- Joules per metre squared (J/m2) is termed ‘Radiant Exposure’
If the exposure time is known then its possible to convert between the two
Determining MPE
For example, imagine a diode laser with a wavelength of 689 nm. It has a power output of 4 mW, a beam diameter of 3mm and is a continuous wave. First the area of the beam is calculated:
From this the irradiance at the laser exit (neglecting divergence) can be calculated:
A more complicated calculation is irradiance to the eyes. The limiting aperture over which the average irradiance for an eye exposure would be 7mm. First the area of the eye aperture is found:
Then the average irradiance to the eye is calculated:
The diode laser emits in the visible range at 689 nm so the blink reflex response needs to be taken into account. At this value the MPE is 18 t0.75 C6 Jm-2. This values is found from a table when t is blink response time of 0.25 s and C6 is the correction factor (this is 1 for our purposes).
Combining all these values the MPE at the cornea works out to be 6.36 Jm-2 or 25.3 Wm-2. These MPE values are clearly exceeded by our previous calculations of 103.9 Wm-2 therefore safety eyewear would be required.
Note: if the laser is invisible, then you can’t use the blink response time of 0.25 s. In this case, 10 seconds is generally used instead.
Nominal Ocular Hazard Distance NOHD
This is the distance from laser aperture at which it would be safe to view the laser without safety glasses, when the laser output is below the MPE level. This can range from ‘cm’ to hundreds of metres and depends on the output level and type of laser. As the beam size gets larger, the area that the power is divided over gets bigger and so the irradiance gets smaller. At a certain distance, the irradiance will equal the MPE and this is called the Nominal Ocular Hazard Distance (NOHD).
Determining NOHD
In order to determine NOHD the following equation is used:
$ NOHD \ (m) \ = \ \frac{\sqrt{\frac{4 \times Power}{\pi \times MPE} \ - \ aperture \ diameter }}{Divergence} $
Radiant power (W), Aperture diameter (m), Divergence (radians), Maximum Permissible Exposure level (Wm-2)
Protective Eyewear
Persons standing at a distance closer than the NOHD should wear adequate protective eyewear. It is designed to reduce worst case accidental viewing conditions to a ‘safe’ level (blink reflex applies). Protection level is reduced when beams are focused to small spot sizes (as encountered in medical applications)
Optical Density
This represents a measure of the transmission of an optical medium for a given wavelength. It is a logarithmic scale:
OD5 results in a reduction in transmission by 105 (100 000 times). OD5 is usually high enough as it reduces a 100 W laser beam to 1 mW.
Note: the optical density fails to explain how long it will offer protection for
BS EN 207(2009)
This takes into account both optical density & damage threshold of a material. This guarantees protection from direct beam for only 5 secs or 50 pulses under specific test conditions. L-number indicates protection level and this varies with mode of operation and wavelength.
| Laser mode | Wavelength range (nm) | Protection Level |
|---|---|---|
| D | 180 - 315 | L10 |
| IR | 180 - 315 | L5 |
| D | 315 - 532 | L6 |
| I | 315 - 532 | L7 |
| R | 315 - 532 | L5 |
| DIR | 1045 - 1100 | L7 |
D - Continuous, I - Pulsed, R - Q switched (v. short powerful pulses)
Laser Interactions
Biological Effects
The interactions that lasers have with biological tissues depend on three main parameters:
- Wavelength Laser radiation needs to be absorbed in tissue to have any effect
- Pulse Duration
- Output Power
The location and level of absorption of laser radiation is strongly wavelength dependent. The interaction effects can be roughly grouped into the following processes:
Photochemical UV blue end
Photochemical damage can occur for lower irradiance that are not high enough to cause thermal damage (i.e. too small to cause a temperature rise). Examples include skin tanning, psoriasis treatment, new born jaundice treatment, sunburn, skin cancer and cataracts.
Thermal
Above a critical tissue temperature, proteins are de-natured and thermally induced damage occurs. At temperatures of 60°C, coagulated tissue becomes necrotic. Once temperatures are greater than 100°C, water in the tissue begins to boil. Further temperature increases lead to carbonisation.
Carbonisation should be avoided since the tissue will die at lower temperatures and it reduces the visibility of a target during surgery. To avoid carbonisation, the tissue is usually cooled using water or gas. Examples of thermal effects include coagulate, cut & burn and heat.
Photoablation thin layers of tissue are removed
On the surface of a tissue such as the cornea for UV and far IR wavelengths, thermo-mechanical effects lead to ablation of material. The heated material is rapidly removed from the rest of the material which is hardly affected by the process.
The depth of tissue removal is determined by the pulse energy. Advantages of this procedure are the precision of etching and the fact that no thermal damage is caused to the surrounding tissue.
UV photons (typically Excimer lasers) provide enough energy for this mechanism to occur. An example of photoablation is vision correction surgery.
Thermomechanical
This occurs when tissue is heated very rapidly. Rapid thermal expansion and vaporisation of liquid leads to mechanical shock waves. Cells rupture explosively.
For ultrashort pulses, a very high temperature plasma may also be formed. This leads to shockwave generation & ablation (a process called photodisruption). Examples of thermomechanical effects include kidney stone removal and removal of fibrous tissue growth which can form after cataract surgery.
Eye Hazards
The eye is the most vulnerable to laser hazards. Injuries can occur at much lower power levels than for the skin and are typically more serious than skin effects:
UVA lens
The lens the pre-dominant absorbed of UV-A although a small amount is absorbed by the cornea. The effectiveness of UV to induce photochemical damage decreases with increasing wavelength. Thermal damage is the main concern here.
UVB cornea lens
UV-B light penetrates deeper into the eye and both the cornea and the lens are at risk. Levels encountered in accidental laser exposure are typically well above the threshold causing permanent damage to the lens.
UVC cornea
The absorption depth is very shallow and all light is absorbed in the surface of the cornea. Exposures above the threshold for damage for short pulses can result in ablation of the cornea .i.e. Excimer lasers.
If the peak irradiance is not high enough for photoablation, inflammation can occur. The injury can take take several hours to develop.
Retinal Damage 400nm - 1400nm
Between 400 nm and 1400 nm wavelengths, the retina is at risk. Transmission is higher in young persons (~380 nm) compared to adults. Concern from widespread use of LEDs emitting in the near UV range. Retinal damage will be permanent.
Infra-red Radiation
Near IR is transmitted to the retina. Mid-range IR affects the cornea and penetrates the aqueous humour. The far IR is absorbed by the cornea.
The cornea is damaged at an irradiance level lower than that necessary to acutely affect the lens. Below 1400nm, injuries can be superficial and will heal within a couple of days. Above 1400nm injuries will be deeper and permanent (well above threshold)
Eye Protection is required to all lasers of class 3R and above.
Skin Hazards
Risk of skin injury is secondary to eye damage. Skin injuries are not as significant and will usually heal, even after penetrating damage that may lead to infections. Damage to the skin may be thermal or photochemical, known simply as a ‘burn’ or a ‘sunburn’. Burn generally means a thermal injury. Sunburn generally means a photochemically induced erythema. Effects on the skin will depend on:
- Power
- Wavelength
- Spot Size
- Duration of Exposure
- Blood Circulation
- Heat Conduction of Exposed Skin
Skin Injuries can vary greatly in severity with a severe thermal injuries possibly damaging the underlying muscle and major blood vessels.
Associated Hazards
Not direct hazards from laser light but the hazards from the equipment that create it, and these include:
- Electrical
- Mechanical
- Chemical
- Fire and Explosion
- Noise
- Temperature & Humidity
- Smoke/Vapour/Fumes
Examples of Laser Applications
- Tattoo Removal: Modern lasers are more gentle and effective at removing tattoos with less chances of scarring.
- Laser Skin Resurfacing
- Ophthalmic Treatments: such as laser vision correction (LASIK treatment)
- Dentistry
- Tongue tumour
- Endovenous Laser Treatment (EVLT)
Written by Tobias Whetton